A Quiet Epidemic
- Zack Boyd
- Aug 6, 2021
- 8 min read
Updated: Sep 10, 2021
Despite the efforts of researchers and organisers, Valley fever remains an obscure disease.

Rob Purdie, a financial worker from Bakersfield, California, woke up on New Year’s Day in 2012 with a headache. It did not go away.
He tried various over-the-counter medications: aspirin, Tylenol. But the pain worsened into a persistent migraine. After a few weeks, he was diagnosed with a sinus infection. Two rounds of antibiotics had no effect, and by February, he was re-diagnosed with cluster headaches.
Soon after, Purdie was giving a presentation for work with his wife. “About halfway through, I started seeing two of everything,” he recalls. After the meeting, his wife drove him to the hospital, where he received a spinal tap and was admitted for nearly a month. He was given a final diagnosis of Valley fever, a fungal infection spread by wind in arid regions of the Americas. He had gotten sick by breathing in dust.
It is impossible to escape dust in California’s San Joaquin Valley, where Bakersfield is situated. During one of the region’s frequent dry spells, dust is as common as the parched grass and citrus groves throughout the Central Valley. Dust is an unavoidable fact of life.
Valley fever, scientifically known as coccidioidomycosis, is caused by two species of Coccidioides fungi, collectively known as cocci (pronounced ‘coxy’) for short. The fungi are found in arid soils across a long swath of the Americas, stretching from Washington state down to Argentina, and between the Pacific Coast and Texas. While in the soil, the fungi flourish during rainy seasons; when the weather warms and water becomes scarce, the filaments become brittle, breaking apart in the wind. Spores can blow as far as 150 miles.
If they are inhaled, these spores become spherules and multiply rapidly, infecting the lungs and causing symptoms of pneumonia. While over half of human cases are mild, even unnoticeable, between one and five per cent spread beyond the lungs. In such severe cases, known as ‘disseminated cocci,’ it is very hard to predict how the body will react. The infection can spread to the skin, resulting in aggressive lesions, infect the bones — potentially causing spinal collapse — or as in Rob Purdie’s case, take hold in the brain. Even with aggressive treatment, roughly 200 patients die of disseminated cocci in the United States every year.
Though Valley fever was first recorded in medical literature in 1892, it wasn’t until the 1930s that the infections were finally connected to a mysterious disease in California’s Central Valley, then called San Joaquin Valley fever. Many refugees from the American Dust Bowl, lacking any immunity from Valley fever, began contracting the disease, giving researchers ample opportunity to study its effects and transmission. Two key discoveries came from this work: the fact that it is nearly impossible for the infection to spread person-to-person, and that patients who recovered were almost never reinfected.
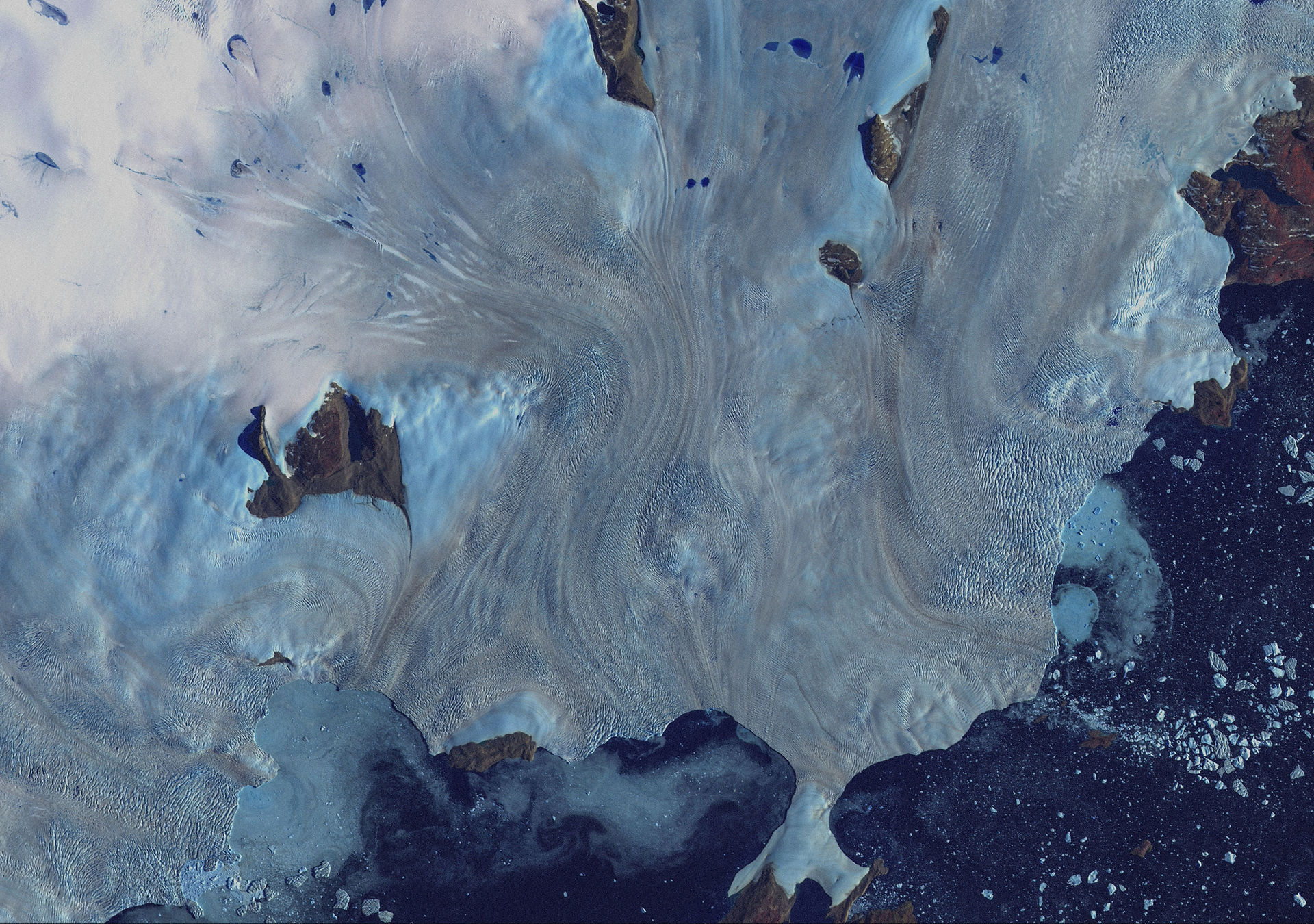
Coccidioides fungal growth in the soil correlates strongly with extreme weather patterns — the fungi’s range could more than triple over the next 100 years.
Despite the fact that well over a century has passed since Valley fever was first medically discovered, there is still a yawning gap in awareness and treatment. According to the Centre for Disease Control and Prevention, over 15,000 cases of Valley fever were confirmed in 2018, more than seven times the number confirmed in 1998. The exact causes of this increase remain uncertain. Still, it is estimated that over 150,000 people contract Valley fever every year in the United States, meaning that well over 100,000 of these cases remain undiagnosed.
Many theories have been proposed to explain the sharp increase in cases, which is outpacing population growth in the American southwest. One of the most likely (and concerning) possibilities lies in the warming climate. Coccidioides fungal growth in the soil correlates strongly with extreme weather patterns, and current climate models suggest the fungi’s range could more than triple over the next 100 years, while also becoming more aggressive in areas where the fungi are already found.
This is not just a theoretical possibility: a 2013 paper demonstrated that the fungus had spread to Washington State and had infected several people. Cocci had previously never been found north of California; the cocci growths in Washington were several hundred miles outside of the known range. Researchers believe that such jumps could become common in the coming decades.
Even though Coccidioides fungi tend to thrive in arid regions, the San Joaquin Valley where it is endemic is one of the most productive agricultural regions in the world, producing crops worth over US$2.5 billion annually. It is also the site of new investment, as the suburbs of Los Angeles stretch ever inland from the Pacific Ocean, reaching up into the Valley. The region’s sunny, open landscape promises a bright future in renewable energy.

Unfortunately, there are downsides to progress. The San Joaquin Valley has some of the worst air pollution in the United States, and much of the agricultural work is made possible by half a million undocumented farm workers, nearly all of whom lack health insurance and basic workplace protections.
The threat of Valley fever only compounds these risks for those who work outdoors. Until only a couple of years ago, there were no state-mandated requirements for training workers on the risk of Valley fever. Lawyer Peter Alfert, who successfully represented five road workers in a US$12 million Valley fever-related case against California’s Department of Transportation in 2014, was shocked at the lack of worker protection at the time. “Companies typically don’t do more than they have to; if Cal/OSHA [the state’s labour regulation branch] isn’t requiring it, they’re not going to do it.” he said.
Alfert’s case is only one of many related to Valley fever (and to date, the most successful). In 2019, the regional federal court ruled on a lawsuit filed by over 100 prisoners at California’s Pleasant Valley Prison. Over a decade earlier, a study had found that inmates at Pleasant Valley were contracting Valley fever at 600 times the local average rate. In 2005, the state eventually evacuated prisoners with compromised immune systems, but prisoners continued to get sick in the following years. The lawsuit filed by the inmates alleged that keeping prisoners in the Central Valley, where a breath of dust could give them a debilitating infection, was a cruel and unusual punishment. The final ruling dismissed these claims; the court ruled that because anybody living anywhere in the Central Valley could get Valley fever, the state did not have to protect its prisoners against it.
Rob Purdie’s current treatment regimen, the most effective for his particular case of Valley fever, begins around 10 o’clock in the morning at the local hospital, 11 if the doctor is running late.
His treatment requires a device called an Ommaya reservoir, implanted under his scalp, which consists of a golf-ball sized port beneath the skin and a tube running through his skull to the centre of his brain. He is given the painkiller Tylenol and anti-allergy medication Benadryl, as well as two anti-nausea medications before the procedure can begin. After disinfecting his scalp several times (“they are careful to avoid infection,” he points out, “it’s a superhighway to the centre of my brain”), a doctor taps his spine to make room in his brain for a single syringe worth of Amphotericin and Posaconazole, pushed directly into his head.
Purdie remembers the first time he received the treatment, “I could feel it moving into my brain, then down through my body… I could feel every muscle tightening up. When it got to the stomach, I could feel my stomach tightening.” A few minutes after treatment, he becomes nauseous, vomits several times, and then enters observation for two hours. He receives this treatment every three months, although most patients that require Ommaya treatment receive it up to three times every week. Even with insurance, each treatment costs $2500.
Purdie’s treatment is not unheard of for Valley fever cases — he knows of roughly 15 other people who receive it at the same hospital — but it is not universal. Some patients require amputation, lifetime dialysis, or any number of other methods to offset the damage done by the infection. Once the spherules are disseminated in the body, there is no cure. Valley fever becomes a lifetime condition that takes over a patient’s life, sometimes in surprising ways: for instance, Purdie’s first antifungal prescription made his skin more sensitive to light. The skin damage from that side-effect has led to six diagnoses of skin cancer before his 50th birthday.
Even in endemic regions, Valley fever is not always tested for, even when patients show symptoms. John Galgiani, director of the Valley Fever Center for Excellence at the University of Arizona, believes this is because many physicians “become doctors outside the endemic region and then come here to practice; they’re clueless because they’ve never seen this disease.” Patients who know about Valley fever are diagnosed quicker than patients who do not, simply because they will ask for a test.
Galgiani and his colleagues at the University of Arizona have been working for nearly a decade on a Valley fever vaccine but have faced considerable obstacles in funding and awareness in the process. For now, they are creating a canine vaccine, on track for approval at the end of 2021, that they hope can pave the way for a human vaccine. Still, the path is not clear, not for lack of research, but because Valley fever is not recognised as a significant issue in the United States.
It is estimated that a human vaccine would require $150-$200 million; current research suggests that the disease causes an economic burden of more than $1 billion every year in California and Arizona alone.
There are economic barriers to the vaccine as well. Without public funding, researchers would have to rely on private investment, and a vaccine for such a locally limited market simply isn’t viable: even if every one of the estimated 150,000 cases per year were confirmed, Valley fever would still be below the threshold of cost-effectiveness, making it an ‘orphan disease’; not enough vaccines could be marketed to make the treatment profitable.
It is estimated that a human vaccine would require $150-$200 million; current research suggests that the disease causes an economic burden of more than $1 billion every year in California and Arizona alone, mainly due to hospital costs, treatments, and loss of productivity.
“It really depends on whether or not this becomes viewed as a public health problem,” Galgiani says. “Making vaccines is a high [economic] risk, and this is a small market. If you have money, you put money where you think you’re most likely to get a return on investment, and we don’t compete well in that paradigm.”
While COVID-19 demands the attention of the world’s medical resources, Valley fever has understandably taken a backseat to the immediate issues of the current pandemic. “The CDC runs on crisis management,” Galgiani observes. “They run to one side of the ship or the other depending on what the crisis is.” As long as Valley fever remains a secondary issue, there will likely never be funding or support to properly mitigate the disease.
Rob Purdie has found some stability in his treatments, and now works as the Patient-Program Development Coordinator at the Valley Fever Institute in Bakersfield. The job has allowed him to advocate for outreach and provide training to key risk groups such as construction workers. The Institute also played a role in supporting a $2 million Congressional grant to the Centers for Disease Control and Prevention for surveillance and awareness, an initiative he hopes will continue in the future.
Awareness will be key to addressing Valley fever in the future. Galgiani believes Valley fever is “simply competing with the many other things to remember. Most people don’t remember things unless they start hearing about it over and over again. Repetition is part of the deal.”
Purdie hopes for a brighter future for those who suffer from the disease. “It’s not just the disease,” he says. “It’s everything that goes with it: the job loss, the family loss, the loss of ability to do the things you used to do in the past, the depression, the emotional aspects.” With more support and more awareness, perhaps future patients can hope for a brighter outlook.
Zack Boyd is a senior at Stanford University, finishing his B.S. in Earth Systems and beginning his M.A. in Environmental Communication concurrently; his main academic interests are environmental justice and sustainable agriculture. He currently lives in Cupertino, California, but is glad he's originally from Kintnersville, Pennsylvania.
Photography: 'Nasty Haze in Central Valley' by rlerdorf is licensed with CC BY 2.0.



Good!
aprw
I was recently looking for a new online casino and stumbled upon rolletto by accident. I really liked the user-friendly interface and the wide selection of games, from slots to sports betting. support and fast payouts make playing comfortable and safe. I'm also happy that they have 24/7 customer support that is always ready to help.