Earth Day: Clinicians and Planetary Health
- Anthroposphere

- May 26, 2019
- 9 min read
By Erika Veidis

Human health, by almost any measure, is better now than at any point in human history. In the last century, we’ve seen average life expectancy more than double and child mortality rates drop to about a tenth of what they used to be. And yet, profound and unprecedented degradation of the natural world threatens to undermine this success. In the face of accelerating global environmental change, we are confronted with new and increasing burdens of disease, declining nutrition, and growing mental health risks. Furthermore, these complex challenges are underscored by questions of equity – despite their limited environmental footprints, the poor, the young, some indigenous populations, and future generations are bearing the brunt of the consequences.
In response to our growing environmental impact and its repercussions on our health, wellbeing, and ultimately survival, many doctors, nurses, and other clinicians around the world are sounding the alarm. Practitioners are saying that protecting health might necessitate expanding beyond clinical walls, which requires engaging in efforts to enact broader change through governmental advocacy, healthcare sustainability, training the next generation to better grasp health-and-environmental linkages, and educating patients about bottom-up action.
“In my own practice, I began to feel a degree of futility taking care of individual patients while the ground was shifting so dramatically under all our feet,” says Dr. Samuel S. Myers, a former internist now serving as Principal Research Scientist in Planetary Health at the Harvard T.H. Chan School of Public Health and Director of the Planetary Health Alliance. “I realized that the majority of disability and death in coming years will be driven by our dismantling of Earth’s life support systems and that understanding and addressing these challenges will be critical to securing human health into the future.”
"In my own practice, I began to feel a degree of futility taking care of individual patients while the ground was shifting so dramatically under all our feet..."
These upstream challenges are rooted in our patterns of production and consumption. In the 1950s, we entered what scientists call “the Great Acceleration,” a period where humanity’s gradually-increasing impacts on ecological systems took a sharp upward turn. This transition has been characterized by rapidly-growing rates of resource use, deforestation, biodiversity loss, pollution, and other aspects of environmental decline. The statistics are oft-cited and staggering: our population has tripled in two generations; a third of Earth’s land surface and three-quarters of its waters are annually appropriated for agriculture; we have dammed more than 60% of rivers and chopped about half of our forests; 90% of global fisheries are exploited at or beyond their maximum sustainable limits; global temperatures are reaching new records; oceans have become 30% more acidic since the Industrial Revolution; 60 billion tons of renewable and nonrenewable resources are extracted globally every year; and 1 million animal and plant species are now threatened with extinction, with an estimated three species lost every hour.
Perhaps even more shocking are the health impacts of environmental change, the subject of a new scientific field called planetary health. Diseases like malaria, dengue, Zika, yellow fever, Lyme, Ebola, and chikungunya are expanding geographically and lengthening in season. The near-quarter decrease in productivity of the Earth’s land surface due to land degradation and the global disappearance of pollinators risks nutrition and livelihoods (with an up to $577 billion USD annual agricultural loss). Further burdening our food systems are increased drought, extreme storms, and atmospheric changes, like the rising carbon dioxide concentrations that directly reduce key nutrients, such as protein, iron, and zinc, in staple crops. The number of reported weather-related natural disasters has more than tripled since the 1960s, resulting in over 60,000 annual deaths, mainly in low- and middle-income countries; this is exacerbated by the loss of coastal habitats, which puts up to 300 million people at increased risk of floods and hurricanes. Industrial emissions and smoke from fires – whether wildfires or human-made fires created to clear forests for agricultural use – can lead to cardiorespiratory illnesses and other diseases. On top of these, witnessing the degradation of our world and contending with the health, economic, and sociopolitical stressors of environmental change isn’t easy, particularly when compounded with decreased contact with nature. This can have severe consequences for mental health in terms of depression, post-traumatic stress disorder, anxiety, and suicide.
"Climate change is a startling reality for the small island developing states of the Caribbean,” says Dr. Paula Henry, a family medicine physician in Trinidad and Tobago. “The increasing intensity of hurricanes and flooding, biodiversity loss, acidification of our oceans, rising sea levels, and the changing face of vector borne diseases has had significant negative impacts on our economy, health, and tourism – the bedrock of many of our territories."
The question of “how did we get here?” has permeated discourse in economic, political, psychological, philosophical, and spiritual realms. Answers usually consist of some combination of short-sighted linear economic models, dissolution of social capital, and profound disconnect from nature, seeing it as an “other” that can be appropriated, hacked, and outsmarted. And the related question – “now what?” – often finds in its response a mix of top-down policy and innovation and bottom-up action.
What bottom-up action looks like is something that doctors, nurses, and other clinicians around the world are trying to address – and as one of the most globally-trusted sources of information, they hold a unique opportunity to move the needle on individual- and community-level change.
“We have to draw the attention of everyone to the fact that we are destroying our planet,” posits Dr. Ifeoma Monye, a family doctor and lifestyle medicine practitioner in Nigeria, where increased flooding, rising sea levels, some of the world’s worst air pollution, and other environmental disruptions are expected to exacerbate existing challenges of disease, food insecurity, and poverty. Monye, who founded the Brookfield Center for Lifestyle Medicine and serves as President of the Society of Lifestyle Medicine of Nigeria, is confident that solutions can be effected through individual action, as encouraged by clinicians: “We have to recognize and question the simple everyday things that we do without a second thought.”
In some cases, clinicians are leveraging their authority as health protectors to advocate for environmental solutions – citing health concerns as reason to fight problematic industrial standards and governmental inaction. The Canadian Association of Physicians for the Environment (CAPE), for example, has been working to decrease the health impacts of pesticide use, air pollution, and fossil fuels, with success in establishing coal phase-out commitments and infrastructure for improved active transport, as well as supporting Canada's new planetary-health-friendly food guide through to its implementation. Courtney Howard, CAPE President and Emergency Doctor, discusses their recent focus on climate and health and reflects on parallels between fighting for patients and fighting for the planet: “I know what it’s like to act too slowly and to have patients die... I also know what it’s like to act quickly, to do the right thing, and to pull someone from the spiral back to where we can thrive.” Doctors and other clinicians, Howard says, are “late to the climate fight” but can utilize their knowledge of saving lives in times of crisis, as well as their status as trusted messengers, to help drive a healthy response to climate change and other threats to planetary health.
Groups similarly invested in directly fighting on issues of environmental change to protect our health include the Global Climate and Health Alliance, the UK Health Alliance on Climate Change, Doctors for the Environment Australia, the Alliance of Nurses for Healthy Environments, and Irish Doctors for the Environment.
What’s new in the latest round of clinically-based action, though, is the integration of mainstream medical and nursing associations and other health-focused organizations into the planetary health movement. Organizations including the World Health Organization (WHO), World Organization of Family Doctors (WONCA), and the World Federation of Public Health Associations (WFPHA) have recently taken stances on planetary health issues, as have prominent national bodies, like the Canadian Medical Association, the American College of Lifestyle Medicine, and the Royal College of General Practitioners, as well as family medicine and public health organizations of the Caribbean, Brazil, Uruguay, the Philippines, Nigeria, Ireland, the United States, and Australia.
This Earth Day saw a broad and unprecedented commitment of the healthcare community to planetary health, with the publication of a global call-to-action in The Lancet, one of the oldest and most prestigious medical journals. Previously, The Lancet had termed climate change “the biggest global health threat of the 21st century,” and with this latest Earth Day feature, the journal highlighted an international array of over 30 healthcare organizations around the world – many of which are listed above – heralding the importance of planetary health. The call-to-action co-signers, partners in a new initiative called Clinicians for Planetary Health, adopted a pragmatic yet urgent tone: We can’t pretend that this is just about the environment anymore; our health is at stake, as is that of future generations.
In the Clinicians for Planetary Health initiative, led by the Planetary Health Alliance, healthcare communities from around the world are banding together to take the next steps in addressing global environmental change. This stitching together of existing efforts and establishment of new collaborative ventures spans the arenas of patient education, university programming, healthcare sustainability, community organizing, and advocacy. Beyond engaging a global array of interested doctors, nurses, and other clinicians with existing opportunities to take action, this collaboration will next focus on developing and disseminating planetary health resources for clinicians and patients. Talking points, informational materials, and other resources will emphasize lifestyle modifications with health and environmental co-benefits – adopting a planetary health diet, choosing active transport, connecting with nature and community – as well as getting involved in local activism. Understanding that planetary health challenges are fundamentally issues of collective action, the Clinicians for Planetary Health initiative seeks to establish clinical communities as the centers of gravity that help provide the information and infrastructure necessary for broader societal change.
This latest surge of activity occurs on the rich foundation laid by previous endeavors. Statements on planetary health – or, more narrowly, climate and health – have been numerous in the healthcare community, as seen in the Lancet-published Australian health professionals' statement on climate change and health, the Global Climate and Health Forum call-to-action, the United States-focused declaration on climate and health, the WHO Director’s commentary on seeing climate change as an opportunity for public health, and the declaration on planetary health distributed by WONCA to its networks of over 500,000 family doctors. New alliances of health organizations devoted to environmental issues have been cropping up across the globe, with increasing recognition that protecting health requires protecting the natural systems on which it depends.
“Evidence-based medicine has become a cornerstone of clinical practice, and the robust research-based field of planetary health extends this by bringing new insights on upstream health challenges and how to treat them,” says Dr. Enrique Barros, a family medicine doctor in Brazil and the Chair of the WONCA Working Party on the Environment. “Soon, clinicians will realize the tremendous co-benefits we can collectively exert on the Earth while giving simple state-of-the-art medical advice to patients, unleashing a powerful wave for social and planetary change.”
The truth, as we well know, is that we have limited time to take action. The recent IPCC report calls for deep cuts in greenhouse gas emissions by 2030 – an almost 50% reduction from 2010 levels – to prevent temperature rises greater than 1.5 degrees Celsius above pre-industrial levels. Exceeding this temperature, they say, would have disastrous consequences in various climate-related economic, sociopolitical, and health risks. Similarly, the IPBES assessment’s alarming reports on the unprecedented, global, and accelerating deterioration of nature and its biodiversity urges us to rapidly alter our course and enact “transformative changes” by 2030 to achieve sustainability goals. In the words of IPBES Chair Sir Robert Watson: “We are eroding the very foundations of our economies, livelihoods, food security, health and quality of life worldwide… it is not too late to make a difference, but only if we start now at every level from local to global.”
Our moment of opportunity to redefine our sense of stewardship of the natural world and avoid the most harrowing predicted effects of our environmental negligence is quickly slipping away. “This is our moment to shine as a species,” Myers argues. “We can chart a course to a carbon-neutral future where human population has stabilized, people are living in cities designed to optimize wellbeing and minimize ecological footprint, our food and manufacturing systems are producing more with fewer inputs and less waste, and there is more breathing room with each passing decade for the rest of the biosphere. Or we can continue a business-as-usual trajectory with dire consequences for humanity and the rest of the biosphere. It is up to us, right now.”
The hope underscoring many of these health-community-based initiatives is that clinicians can lead the change and help overcome the barriers of collective action that thwart other movements – lack of information, lack of infrastructure, lack of leadership, lack of interpersonal trust, and excessive perceived personal sacrifice. Doctors, nurses, and other clinicians are powerfully positioned to provide guidance backed by the authority of a clinical degree, encourage patients to pursue behaviors that are beneficial for their health and wellbeing, and facilitate local-to-global translations and collective action through leveraging extensively-networked healthcare systems and professional societies. In doing so, health professionals can protect not only the health of their patients, but help to heal a broken planet.
Erika Veidis serves as the Member Engagement and Outreach Manager of the Planetary Health Alliance, which works with a global consortium of over 150 universities, non-governmental organizations, research institutes, and government entities in advancing research, education, policy, and public outreach efforts focused on understanding and addressing the health impacts of global environmental change. Erika graduated from Harvard University with a B.A. in Government and Mind/Brain/Behavior and received an M.B.A. from the California Polytechnic State University. She has had experience across a range of topics, including political insecurity and governance, social movements, environmental economics, and conservation.
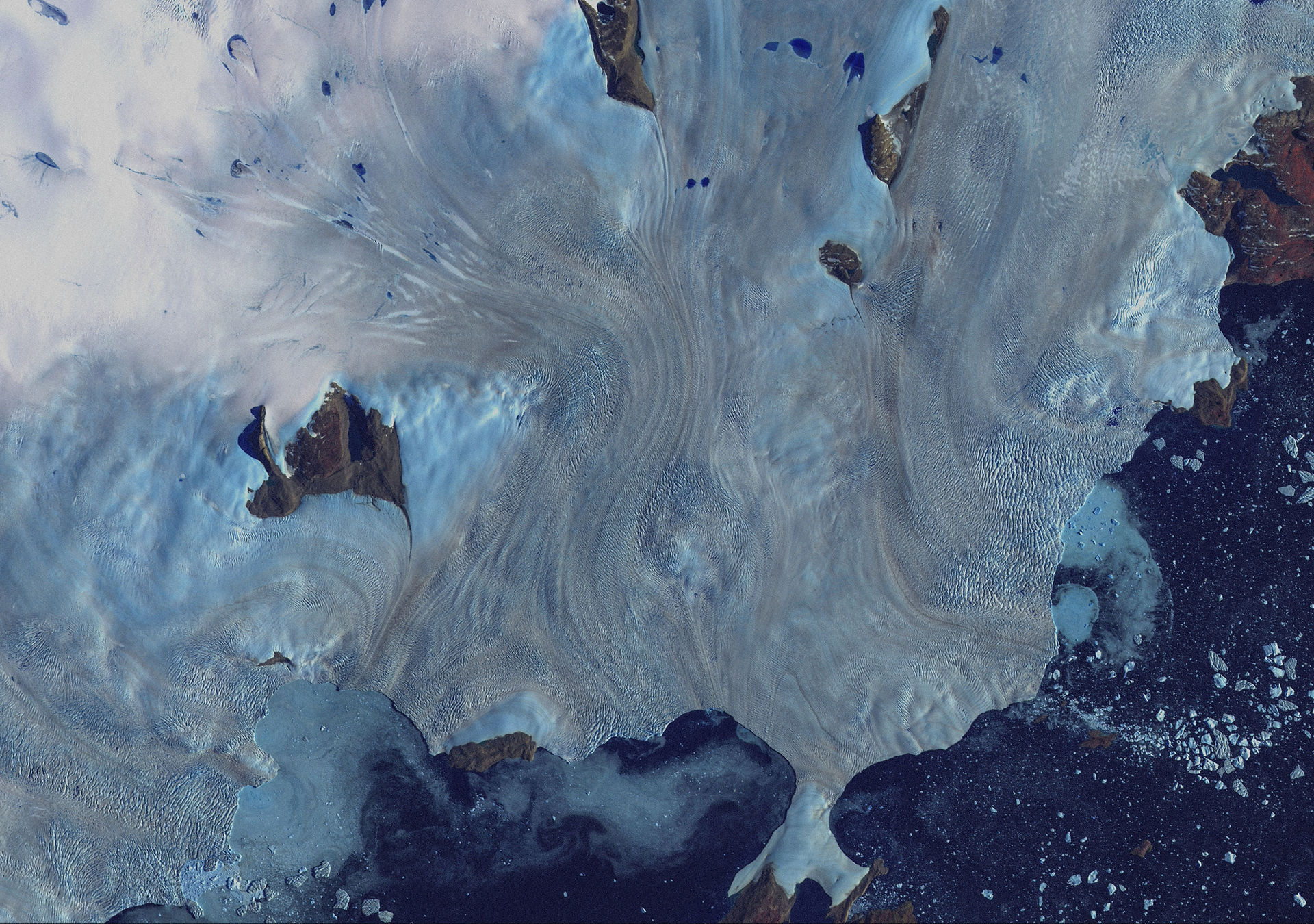
Art by Kristian Hallet
If you like what you've just read, please support Anthroposphere by buying one of our beautifully designed physical copies here. All proceeds go towards printing, designing and maintaining our publication, and your contributions will help keep our climate journalism interdisciplinary and accessible for all.



Comments